What Exactly Is GERD?
What exactly is gerd?What is GERD? Heartburn or indigestion can occur at any time. Around 20% of adults in the United States experience heartburn or acid reflux. However, if it happens more than twice a week, a person may have Gastroesophageal Reflux Disease (GERD). GERD, also known as acid reflux, is a widespread disease of the digestive system. GERD affects at least 1 in every five adults in the United States. However, the real number of people who suffer from GERD is unknown as many people with the symptoms do not seek care from a healthcare provider.
Over five million people were hospitalized for GERD during 2010, with 1653 deaths from the disease. Rates of GERD in infants and children are also rising, increasing 42% for infants and 84% for children between ages 2 and 17 between 1998 and 2005.
GERD is a long-term, or chronic, condition that causes stomach acid to regurgitate into the esophagus. The esophagus is a tube that connects your stomach and throat and is linked by a moist tissue called the mucosa. Its primary function is to carry food and liquid from your mouth to your stomach. GERD can lead to permanent damage to the esophagus if not treated.
What Causes GERD? The esophagus has two sphincters that open and closes depending on whether a person is eating, belching, breathing, or vomiting. These two sphincters are the upper esophageal sphincter (UES) and the lower esophageal sphincter (LES). The UES is located at the top of the esophagus and prevents food and secretions from entering the windpipe. The LES prevents stomach contents and acid from regurgitating from the stomach. The UES is voluntary, while the LES is involuntary.
GERD is the result of a weak LES that causes inadequate closure. The LES acts as a gatekeeper; it opens when you swallow, allowing food to pass into your stomach and then, in an ideal world, closing to prevent the contents of your stomach from coming back up. Refluxing occurs when those contents in your stomach travel backward from the stomach due to the LES's inability to fully close.
When this happens, people with GERD may experience a burning sensation from mild soreness to extreme burning. The lining of the esophagus is very susceptible and can easily be irritated by anything that might have been in your stomach. Reflux of stomach acid can cause a weakening of the cells that make up the lining of the esophagus. This can cause a syndrome known as Barrett's esophagus. Reflux can also cause inflammation in the esophagus, leading to esophagitis. 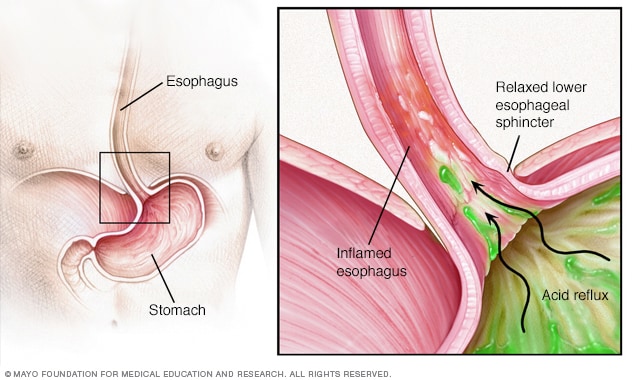 Photo Mayo Clinic
Symptoms There are many symptoms of GERD. GERD symptoms can include chest pain, regurgitation, heartburn, breathing problems, bad breath, and the erosion of teeth enamel. GERD can happen at any age but is more likely to occur in older adults and pregnant women.
Stomach acid can irritate the throat and vocal cords. This can cause a chronic, dry cough or hoarseness. Difficulty swallowing or a sore throat may also occur from this irritation. A person may find themself continually clearing their throat or the sensation of a lump in their throat that they cannot clear. Their throats may feel raw. Additionally, choking episodes may occur if the issue is severe enough.
Breakdown of the enamel of teeth is caused by acid reflux, in addition to bad breath, and dry mouth. Water brash, when the mouth floods with saliva, is also caused by GERD. Inflammation of the gums, a crawling sensation in the mouth, and a burning sensation within the mouth have been noted by those suffering from GERD.
GERD can be difficult to diagnose in children and infants because they cannot tell a parent or other adult what symptoms they may be having. However, the symptoms can differ from those in adults. Children may demonstrate repeated vomiting, coughing, continual spitting up, or respiratory problems. These respiratory problems might manifest in wheezing. Additionally, an infant may appear inconsolable during and after feedings or may refuse food altogether. They may have poor weight gain, bad breath, and belching. Children may also display no symptoms at all.
Risk Factors Many Americans are living with the risk factors for GERD. Risk factors are variables that are present in a person that increases the likelihood of developing a medical condition. It is important to note that these are not what causes GERD, but what can increase the possibility of creating a medical condition later. There are many risk factors for GERD.
Many medications are associated with higher rates of GERD. These medications are used to treat other conditions but unfortunately develop conditions that increase the possibility of GERD. Medications used for conditions like asthma, depression, high blood pressure can increase the risk.
If a patient has a hiatal hernia, their chances of developing GERD also increase. A hiatal hernia happens when part of the stomach presses up into someone’s diaphragm, causing the stomach to become tighter and tighter. It is believed that this might cause weakness in the LES. This allows for stomach acid to more easily reflux into the esophagus. Pregnancy and obesity also place more pressure on the stomach than usual.
If someone smokes, this can weaken the LES. This happens from the nicotine in the tobacco relaxing the LES, causing the stomach acid and contents to reflux back into the esophagus. Smoking also results in a reduction of saliva, which is responsible for neutralizing acid in the stomach. Smoking stimulates acid production in the stomach, increasing the risk for stomach acid to regurgitate through the weakened LES. Often, smokers who complain of GERD symptoms will see a reduction in occurrences and intensity after they quit smoking.
Any condition that weakens the esophageal muscles can lead to GERD in the future. This can also be seen in smokers as the nicotine also relaxes the muscles of the esophagus, making it easier for stomach acid to rise up the esophagus. Weak esophageal muscles make it easier for stomach acid and contents to reflux back into the esophagus, causing GERD symptoms.
Diagnosis There are a few ways the medical providers diagnose GERD. Based on your symptoms, your medical provider may recommend medical tests like upper endoscopy, ambulatory acid (pH) probe test, esophageal manometry, or x-ray of your upper digestive system.
An upper endoscopy is a procedure where the doctor uses s flexible tube with both a light and a camera and then inserts it down your throat. This allows the doctor to visualize the inside of both your esophagus and your stomach, looking for signs of GERD. It is not a definitive test for GERD if the acid reflux is present; however, this medical test can help show inflammation in both the esophagus indicated repeated reflux. During the endoscopy, the physician can also take a biopsy of the tissue within the esophagus for further testing. The biopsy from this procedure could show signs of complications from GERD.
An ambulatory acid probe test is an outpatient procedure that uses a monitor placed into the esophagus. This monitor then identifies when and for how long stomach acid has refluxed into the esophagus. During this test, you will wear a small computer that attaches to your waist and receives the messages from the monitor in your esophagus. This monitor stays in place for only 24 hours. It monitors for GERD signs and can also be used to identify if current treatment measures are working to reduce GERD.
Esophageal manometry studies the muscle contractions in the esophagus. Because GERD can result from a weakened LES and relaxation of the muscles of the esophagus. Manometry studies the contraction your esophageal muscles make while swallowing as well as how coordinated those muscles are.
Medical providers will also take an x-ray of your upper digestive system. It requires you to drink a thick, chalky liquid called contrast so that the radiologist can get a better view of all the organs on the x-ray. This contrast coats all of the organs of the upper digestive tract casting a silhouette on the x-ray. This x-ray can show damage from GERD.
Complications of GERD GERD also has many concerning complications like Barrett’s esophagus, esophageal strictures, and esophagitis when left untreated. People with GERD can also develop respiratory issues like asthma, sinusitis, acid regurgitation into the lungs.
Barrett’s esophagus occurs when there is damage to the esophagus’ lining, like repeated stomach acid exposure from reflux. This disorder is present in roughly 8% to 15 percent of people with GERD. It can cause even more frequent heartburn, difficulty swallowing food, chest pain, and coughing. Having Barret’s esophagus also increases the risk of developing esophageal cancer.
Esophageal strictures occur when narrowing of areas of the esophagus occurs. It can cause a condition known as dysphagia, when it becomes difficult to swallow. Esophageal strictures occur when the acid reflux from GERD causes inflammation to the esophagus, scaring it and making it lose its elasticity.
Esophagitis is the inflammation of the mucosa of the esophagus. Stomach acid frequently backs up into the esophagus, leading to long-term inflammation. This condition can cause difficulty swallowing, like esophageal strictures, but also has a sore throat or heartburn. It can even cause chest pain.
Treatment of GERD GERD has many treatments, but their indication changes depending on how severe the symptoms become. Doctors will almost always begin the plan of treatment with conservative measures. These include lifestyle changes, medication, or surgery.
Before progressing to more invasive treatment options like surgery or medications, your medical provider will most likely want to attempt lifestyle changes or other non-medical treatments. You may be suggested that sleeping with your head elevated will help your GERD symptoms. Sleeping with your head raised prevents the backup of stomach acid while you are sleeping. A bed wedge is one of the easiest ways to sleep with your head raised without discomfit. These devices come as a foam or inflatable bed wedge to position someone in the correct position to prevent reflux. People suffering from GERD may find it beneficial to invest in a travel wedge pillow to prevent GERD symptoms from appearing during travel or when a sufficient number of pillows is unavailable to help keep the head raised.
Medical providers will also suggest other lifestyle changes. These include maintaining a healthy weight, smoking cessation, and diet changes. Smoking is known to weaken the LES, relax the muscles in the esophagus, and increase stomach acid production. All these can make GERD worse. People that suffer from GERD are instructed to avoid fried, fatty, or acidic foods that can trigger reflux. They will also be recommended to avoid wearing tight-fitting clothing that might put more pressure on their LES and lower abdomen, increasing the chances of reflux.
However, they may recommend over-the-counter or prescription medications to help lessen the symptoms or conditions that make GERD continue. Over-the-counter medications include antacids, H-2 receptor blockers, or proton pump inhibitors. Antacids help to neutralize stomach acid providing quick relief to GERD symptoms. H-2-receptor blockers help reduce acid production in the stomach. Proton pump inhibitors block the production of acid in the stomach while also healing the esophagus. Prescription medications for GERD
Surgery is often the last treatment option when all other conservative options have failed. These surgical options include fundoplication, installation of a LINX device, or transoral incisionless fundoplication. During fundoplication, a surgeon will wrap the top of the stomach around the LES, tightening it to prevent reflux. This procedure is a minimally invasive procedure, usually laparoscopic, and can be a complete or partial fundoplication. When a LINX procedure is performed, a ring of magnetic beads is wrapped around the junction between the stomach and esophagus. These beads help keep this junction closed, reducing acid reflux through the magnetic attraction between the beads. Transoral incisionless fundoplication (TIF) is a procedure to strengthen the LES by wrapping part of the stomach around the LES using polypropylene fasteners. As the name implies, there is no surgical incision with this procedure. Instead, everything is performed through the mouth. It has a speedy recovery time and is much less invasive than the regular fundoplication.

|